Source: Cancer Quest
Overview of Metastases
The majority of deaths (about 90%) associated with cancer are due to the metastasis of the original tumor cells to sites distant from the initial or primary tumor. Metastasis is the process by which cancer cells migrate throughout the body.
In order for cells to move through the body, they must first climb over/around neighboring cells. They do this by rearranging their cytoskeleton and attaching to the other cells and the extracellular matrix via proteins on the outside of their plasma membranes. By extending part of the cell forward and letting go at the back end, the cells can migrate forward. The cells can crawl until they hit a blockage which cannot be bypassed. Often this block is a thick layer of proteins and glycoproteins surrounding the tissues, called the basal lamina or basement membrane. In order to cross this layer, cancer cells secrete a mixture of digestive enzymes that degrade the proteins in the basal lamina and allow them to crawl through.
The proteins secreted by cancer cells contain a group of enzymes called matrix metalloproteases (MMP). These enzymes act as ‘molecular scissors’ to cut through the proteins that inhibit the movement of the migrating cancer cells. Once the cells have traversed the basal lamina, they can spread through the body in several ways. They can enter the bloodstream by squeezing between the cells that make up the blood vessels.
Once in the blood stream, the cells float through the circulatory system until they find a suitable location to settle and re-enter the tissues. The cells can then begin to grow in this new location, forming a new tumor.
The process of metastasis formation is very inefficient process but leads to the majority of deaths associated with cancer. This is because the number of cells that leave a tumor can be in the millions per day. Even if only a small fraction of the cells that leave a tumor are able to survive to form a new tumor, the large number of attempts means that a distant growth is likely to occur at some point
Migrating cancer cells can die from a variety of causes, including:
- Cells normally live tightly connected to their neighbors and the meshwork of proteins surrounding them. Detachment from the surface of other cells can lead to cell death (called anoikis ‘an-oh-e-kus’).
- Cancer cells are often quite large in comparison to the cells that normally live in the lymphatic system or blood system. When they travel through the vessels they can get damaged or stuck, leading to cell death.
- Cancer cells can be recognized and destroyed by cells of the immune system
Additionally, it is important to note that even if a cancer cell does not die, it does not mean that it will form a tumor. The cells may exist at locations far from the original tumor without multiplying enough to cause any problems.
Watch Emory Winship Cancer Institute Researcher Adam Marcus describe his research on cancer metastasis. Contains actual video of cancer cells moving.
Formation of Metastases
Colony Formation
A metastatic tumor cell must successfully “set up shop” in a new organ to form a secondary tumor, this process is termed colony formation. The metastatic cell must create favorable surroundings within a hostile foreign environment that will allow for their growth and survival. This appears to be the make or break step in metastasis. In an experimental model of metastatic melanoma, more than 80% of injected cancer cells survived in the circulation and exited to the liver. Of these, only 1 cell out of 40 formed micrometastases within 3 days, and of those only 1 cell in 100 formed macrometastases within 10 days. Creating a friendly environment appears to be a difficult process that limits a metastatic cell’s ability to form a secondary tumor.3
Obstacles to Colony Formation
What makes colony formation such an inefficient step? The surrounding tissue (stroma) of the new organ will be very different from that of the original site and in most cases will be unfriendly to tumor cell survival. If the metastatic cell cannot change the new stroma into a more friendly environment, it will not successfully colonize the new site (for example, promote angiogenesis), and a secondary tumor will be unable to form.4In these cases the tumor cells are said to be dormant: they do not die, but they are incapable of growing. Aquisition of additional mutations often allow these dormant micrometastases to overcome the difficulties they face in new tissues and to successfully colonize it, forming a true metastatic tumor. 5
Routes of Metastasis
There are three primary ways tumors can spread to distant organs:
- Through the circulatory (blood) system (hematogenous)
- Through the lymphatic system
- Through the body wall into the abdominal and chest cavities (transcoelomic).
The circulatory system is the primary route of spread to distant organs, while lymphatic vessels provide a route to local lymph nodes, after which metastases often travel through the blood 4While the circulatory system appears to be the most common route, the extent of lymphatic versus hematogenous spread appears to depend on the origin and location of the primary tumor.6For example, bone and soft tissue tumors (sarcomas) spread primarily through the blood, while melanoma, breast, lung and gastrointestinal tumors spread through the lymphatic system.7Transcoelomic spread is fairly uncommon, and appears to be restricted to mesotheliomas and ovarian carcinomas.8
In order for tumor cells to gain access to lymphatic or blood vessels, tumors need to promote the growth of these vessels into and around the tumor. Growth of blood vessels is called angiogenesis, and growth of lymphatic vessels is lymphangiogenesis.
The Lymphatic System
The lymphatic system plays an important role in controlling the movement of fluid throughout the body. Specifically the lymphatic system controls the flow of lymph, a colorless fluid containing oxygen, proteins, sugar (glucose) and lymphocytes (cyte=cell). There are some similarities and differences between the (more well known) circulatory system and the lymphatic system.
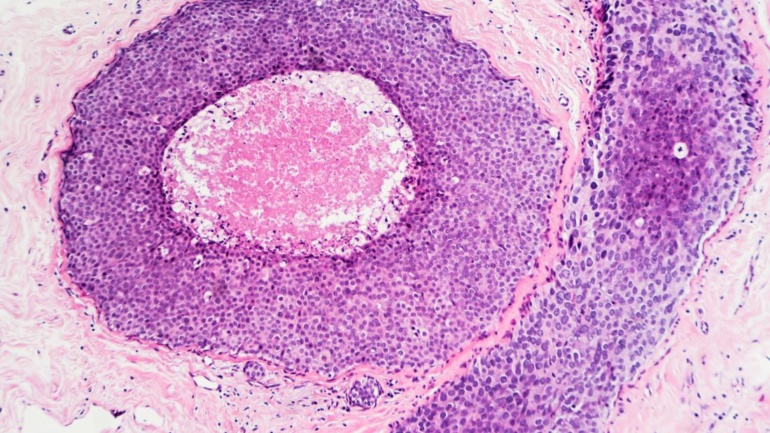
Small lymphatic vessels merge into larger ones and these large vessels eventually empty into lymph nodes. Lymph nodes are kidney bean shaped tissues that are found in grape-like clusters in several locations around the body. Lymph nodes are sites of immune system activation and immune cell proliferation (growth). The fluid in this extensive network flows throughout the body, much like the blood supply. It is the movement of cancer cells into the lymphatic system, specifically the lymph nodes, that is used in the detection of metastatic disease. The staging of cancer is discussed in more detail in the Diagnosis and Detection section.
The Anatomic Model
In the anatomic model of metastsis, secondary tumors occur in the organs which they encounter first during their dissemination from the primary tumor. This scenario appears to occur in regional metastases, where tumor cells gain access to nearby tissue or lymph nodes through the blood or lymphatic circulation. 9For example, liver metastasis is a major occurrence in patients with colorectal cancer. In this case, the capillary bed of the liver is the first encountered by the tumor cells after leaving the colon, and the liver seems to provide a suitable environment for the growth of these secondary tumors. 3However, metastasis to distant organs occurs through a different mechanism (see next section).
The Seed and Soil Hypothesis
Early cancer researchers noticed a propensity for certain cancers to metastasize to the same organ. In 1889 Stephen Paget observed that patients with breast cancer often developed secondary tumors in the liver. He considered it unlikely that this occurrence was due primarily to accessibility of the liver by the blood supply, as other organs receiving equivalent blood supply rarely developed metastases. He instead developed the “Seed and Soil” hypothesis, in which certain tumor cells (the seeds) can only successfully colonize selective organs (the soil) that have suitable growth environments 10
The current view of the Seed and Soil Hypothesis consists of three important concepts.
- Primary tumors and their metastases consist of genetically diverse tumor and host cells (for more on the role of the host cells in cancer, see the section on Tumor Microenvironment).
- Metastasis selects for cells that can succeed in all phases of the metastatic process. In essence, a successful metastatic cell must be a decathalete: good in all the events, and not just one or two.
- Metastases generally develop in a site specific way. Because the microenvironments (the soil) of each organ is different, individual cancer cells may be able to colonize one specific organ.9
At the heart of the Seed and Soil hypothesis is the idea that successful metastasis depends on the interaction of the metastasizing tumor cells with the cells of the target organ (the stroma, or tumor microenvironment). Not only must tumor cells must be able to produce factors that alter the stromal cells in such a way as to better serve the survival and growth of the tumor, but the environment in which the cancer cell finds itself must be capable of responding to those signals. If the cancer cell finds itself in an inhospitable soil (i.e. it cannot subvert the stroma to serve its needs), successful metastsis will be impossible. 4
Recent studies examining the profile of genes expressed in tumors that metastasis to specific organs have identified specific genetic signatures of these tumors. For example, genes that mediate the metastasis of breast cancer to bone are different than those that mediate metastasis to the lung. In essence, different sets of genes allow tumor cells to specifically interact with the stromal cells of the target organ. These findings may lead to therapeutic strategies to target the metastatic properties of tumors.11
How Metastases Form New Tumors
Barriers to Metastasis
In certain cases tumor cells invade a foreign tissue, but fail to colonize it; in effect, they remain dormant. What causes the inability of these cells to successfully establish secondary tumors? They may be incapable of promoting sufficient angiogenesis, or they may be unable to reproduce, either of which might be due to a lack of the proper interactions between the tumor cell and its new environment. Additional mutations appear to be required for these cells to overcome the difficulties encountered in new tissues5
Dissecting the interactions of the tumor and its environment is very challenging. The vast number of growth factors, cytokines, and other factors present, as well as the many signaling pathways involved in cross-talk between these two entities makes mechanisms difficult to unravel, and almost any outcome is seemingly possible. However, the importance of the tumor microenvironment is now very obvious, and as more is learned about it, greater numbers of therapeutic strategies targeting the environment alone or in conjunction with the tumor itself will become available.
Learn more about tumor-host interactions.
Drugs That Target Metastasis
Metastatic Suppressors
Recent work has uncovered a group of molecules that act to induce or suppress metastasis without affecting the growth of the primary tumor. Many molecules, termed Metastatic Suppressors, have been identified. These molecules are critical for different stages of metastasis, and may function to inhibit cell death upon loss of cell adhesion, or enhance the ability of cells to migrate through the stroma. Researchers are hopeful that these molecules may prove valuable as anti-cancer/anti-metastasis targets.12
It is important to realize that the majority of current anti-cancer drug studies are conducted using primary or cultured tumor cells, and the efficacy of each drug is measured by its ability to reduce the size of primary tumors or kill cells being grown in laboratories. However, because metastatic suppressors do not affect growth of the primary tumor, it is likely like many potentially useful anti-metastatic drugs have been overlooked. New methods of analyzing the ability of drugs to inhibit metastasis, rather than primary tumor growth, are being developed, and should lead to a useful new class of therapeutic compounds.3
Anti-angiogenesis Therapy
Because metastasis relies on the growth of new blood vessels in both the primary and secondary tumors, drugs that inhibit angiogenesis may inhibit metastasis. Currently, the combination of anti-angiogenesis drugs with chemotherapy/radiation is the most effect treatment. Unfortunately, many tumors become resistant to the anti-angiogenesis treatment, so this is generally not a longterm solution. 5
Current research into inhibiting metastasis is focusing on understanding which step of metastasis is the most amenable to therapy. The identification of metastatic suppressor genes has opened up many exciting new potential targets for preventing and inhibiting this deadly event.
Challenges to the Development of Anti-metastasis Drugs
Finding potential drugs that block metastasis is difficult, but getting those drugs evaluated in humans can be even more difficult. Most clinical trials are designed to find out if drugs can kill cancer cells or prevent tumors from growing. A drug that prevents metastasis may not show either of these two activities. Some researchers feel that it is important to come up with new kinds of clinical trials that would specifically look at the ability of drugs to prevent the spread of cancer.13
Section Summary: Metastasis
Metastasis
- Metastasis is the process by which cancer cells spread to distant locations in the body.
- The majority of death associated with cancer is due to the metastasis of the original tumor cells.
- Metastasizing cancer cells must secrete a mixture of digestive enzymes in order to degrade barriers.
- Cancer cells may use the circulatory system to move to a suitable location to settle.
- Metastasis is a very inefficient process. Most cancer cells die once they leave the original tumor.
Lymphatic Metastasis
- Cancer can use the lymphatic system as well as the circulatory system to metastasize.
- The movement of cancer cells via the lymphatic system into lymph nodes is used in the detection of metastatic disease and tumor staging.
Some cancers may spread through direct contact with other organs, as in the gut cavity. Metastatic tumors often interfere with the functions of affected organs.
- 1.Urry, L. A., Cain, M. L., Wasserman, S. A., Minorsky, P. V., & Reece, J. B. (2017). Campbell Biology (11th ed.). Pearson.
- 2.
- 3.a. b. c. Steeg, P.S. 2006. Tumor metastasis: mechanistic insights and clinical challenges. Nat Med. 12:895-904. [PUBMED]
- 4.a. b. c. Bacac, M., and I. Stamenkovic. 2008. Metastatic cancer cell. Annu Rev Pathol. 3:221-47. [PUBMED]
- 5.a. b. c. Gupta, G.P., and J. Massague. 2006. Cancer metastasis: building a framework. Cell. 127:679-95. [PUBMED]
- 6.Gerhardt, H., and H. Semb. 2008. Pericytes: gatekeepers in tumour cell metastasis? J Mol Med. 86:135-44. [PUBMED]
- 7.Kopfstein, L., and G. Christofori. 2006. Metastasis: cell-autonomous mechanisms versus contributions by the tumor microenvironment. Cell Mol Life Sci. 63:449-68. [PUBMED]
- 8.Tan DS, Agarwal R, Kaye SB. Mechanisms of transcoelomic metastasis in ovarian cancer. Lancet Oncol. 2006 Nov;7(11):925-34. [PUBMED]
- 9.a. b. Fidler, I.J. 2003. The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev Cancer. 3:453-8. [PUBMED]
- 10.Paget, S. 1889. The distribution of secondary growths in cancer of the breast. The Lancet. 1:571-573. [PUBMED]
- 11.Minn, A.J., G.P. Gupta, P.M. Siegel, P.D. Bos, W. Shu, D.D. Giri, A. Viale, A.B. Olshen, W.L. Gerald, and J. Massague. 2005. Genes that mediate breast cancer metastasis to lung. Nature. 436:518-24. [PUBMED]
- 12.Stafford, L.J., K.S. Vaidya, and D.R. Welch. 2008. Metastasis suppressors genes in cancer. Int J Biochem Cell Biol. 40:874-91. [PUBMED]
- 13.Steeg P.S. 2012. Perspecitives: The Right Trials Nature 485, S58-S59 [https://www.nature.com/nature/journal/v485/n7400_supp/full/485S58a.html]