Early detection helps save lives. Help decrease your risk of developing cancer by using the below AFCR Early Cancer Detecion Guide.
| AGE | FREQUENCY | FEMALES | MALES |
|---|---|---|---|
| 18 – 20 | One Time | Complete health exam1 | Complete health exam1 |
| Yearly | No action needed | No action needed | |
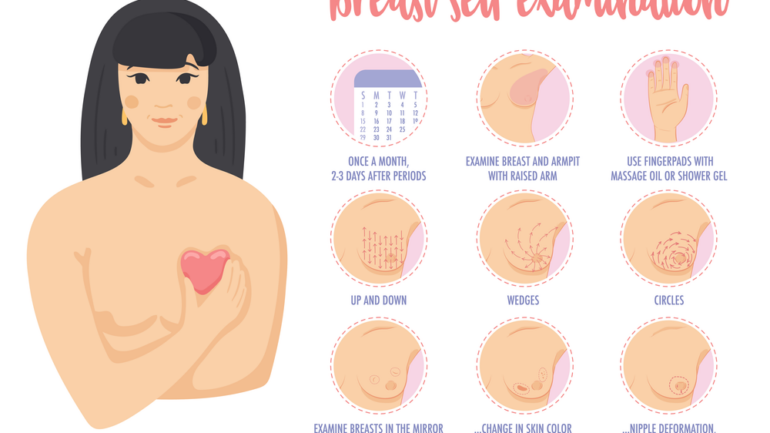
| Monthly | Skin self-exam | Skin self-exam, testes self-exam | |
| 21 – 39 | Every 3 years | Complete health exam1, clinical breast exam, Pap test2 | Complete health exam1 |
| Yearly | Endometrial biopsy3 | No action needed | |
| Monthly | Skin self-exam, breast self-exam | Skin self-exam, testes self-exam | |
| 40 – 49 | Every 3 years | Complete health exam1, Pap test2 | Complete health exam1, prostate-specific antigen (PSA) blood test4 |
| Yearly | Clinical breast exam, mammogram, pelvic exam, digital rectal exam, endometrial biopsy3 | Digital rectal exam | |
| Monthly | Skin self-exam, breast self-exam | Skin self-exam, testes self-exam | |
| 50 – 65 | Every 5-10 years | Colonoscopy, flexible sigmoidoscopy, double contrast barium enema (DCBE)5 | Colonoscopy, flexible sigmoidoscopy, double contrast barium enema (DCBE)5 |
| Every 3 years | Pap test2 | No action needed | |
| Yearly | Complete health exam1, clinical breast exam, mammogram, endometrial biopsy and/or transvaginal ultrasound3, pelvic exam, digital rectal exam, fecal occult blood test (FOBT) or fecal immunochemical test (FIT)5, low dose helical CT (LDCT)6 | Complete health exam1, prostate-specific antigen (PSA) blood test4, digital rectal exam, fecal occult blood test (FOBT) or fecal immunochemical test (FIT)5, low dose helical CT (LDCT)6 | |
| Monthly | Skin self-exam, breast self-exam | Skin self-exam, testes self-exam | |
| 65+ | Every 5-10 years | Colonoscopy, flexible sigmoidoscopy, double contrast barium enema (DCBE)5 | Colonoscopy, flexible sigmoidoscopy, double contrast barium enema (DCBE)5 |
| Yearly | Complete health exam1, clinical breast exam, mammogram, endometrial biopsy and/or transvaginal ultrasound3, pelvic exam, digital rectal exam, fecal occult blood test (FOBT) or fecal immunochemical test (FIT)5, low dose helical CT (LDCT)6 | Complete health exam1, prostate-specific antigen (PSA) blood test4, digital rectal exam, fecal occult blood test (FOBT) or fecal immunochemical test (FIT)5, low dose helical CT (LDCT)6 | |
| Monthly | Skin self-exam, breast self-exam | Skin self-exam, testes self-exam |
1. At minimum, includes medical/lifestyle history and physical exam. Blood/urine tests and chest x-ray may also be included, at physician’s discretion.
2. Women 21-29 should have a Pap test every 3 years, even if vaccinated for HPV. Women 30-65 should have HPV and Pap co-testing every 5 years or Pap test alone every 3 years. Women aged 65+ should stop cervical cancer screening all regular screening results were negative for the past 10 years. Women who have had a total hysterectomy for reasons unrelated to cancer do not require Pap or HPV screening.
3. Beginning at age 35, for women at high risk for endometrial cancer only. This especially includes women with genetic mutations associated with hereditary nonpolyposis colon cancer (HNPCC). Women with HNPCC who have finished having children may choose to have a hysterectomy.
4. Research has not yet proven whether the benefits of prostate cancer screening outweigh the harms of testing and treatment. All men should talk with their doctor to decide if testing is right for them, beginning at age 50 for men at average risk and at age 40 for men at high risk. For men who decide to be tested, the frequency will depend on their PSA level.
5. Beginning at age 50, men and women should take one of the following examinations: Colonoscopy (every 10 years), Double-contrast barium enema (every 5 years), Flexible sigmoidoscopy (every 5 years), or FOBT or FIT, with at least 50% test sensitivity for cancer (yearly). Screening with the FOBT/FIT should be done at home, using multiple-sample method.
6. Lung cancer screening should only be considered for persons who meet all of the following criteria: Aged 55-74, in fairly good health, have a 30 pack-year smoking history, and either still smoke or quit within the past 15 years. Screening should only be done at facilities that have experience in LDCT for lung cancer screening. Discuss risks and benefits with your physician to decide if screening is right for you.
Note: Your doctor may suggest a different testing schedule depending on your risk of developing a specific type of cancer. Discuss with your doctor to develop a screening schedule that is tailored to your own situation.